How might we improve patient and staff experiences at an outpatient hospital clinic?
The Challenge
How might we identify human-centered design interventions that will improve patient and staff experiences at an outpatient hospital clinic?
The Solution
The identification of six research-informed human-centered design (HCD) projects that would improve patient and staff experiences.
The Impact
Clinic leaders hired our design organization to implement two of the proposed projects and presented our findings at their departmental retreat.
Time: 5 weeks, Summer 2022
Sector: Healthcare
Client: University of Illinois Health (UI Health) + Institute for Healthcare Delivery Design (IHDD)
My role: Design researcher and strategist
Services:
Research planning
1:1 interviews
In-context observations
Analysis + synthesis
Presentation of findings
Pilot proposal
What makes this project unique?
The clients for this project (several leaders of the hospital clinic) had not encountered human-centered design before, so were understandably wary of paying a high consulting fee for an untested method. As a result, this five-week exploration was offered pro-bono. At the conclusion of the project, they was impressed enough with the project proposals to hire our design organization to complete the next phase of work. This was meaningful as both an endorsement of our work as well as the power of HCD.
1. Challenge
Project goals
1. Understand the current appointment experience from clinician, staff and patient perspectives.
2. Identify barriers to a positive, productive, and effective work environment and culture for clinic personnel.
3. Understand challenges faced in one specific clinic in achieving desired patient volume.
2. Research + Insights
Key insights
1. Disjointed systems erode staff trust in clinic systems and each other.
I always clear out my box, but it takes four days [for messages] to get in. The patient doesn’t know that, they just know I haven’t responded in four days. — Physician
2. Lack of trust between staff corrodes opportunities for more effective collaboration.
If you’re saying, ‘Can I help you?’ people think you’re saying they can’t do their job. But if you say ‘Can you help me?’ people think you’re being lazy. — Medical Assistant
3. Institutional barriers reduce faith in initiatives for improvement
I asked a lot when I first started, and people just keep saying, ‘Oh, it's just how it is. It's been this way for years. The union dictates schedules and like nothing can be done. Just, like, don't even try.’ — Physician
Reframing the challenge
Lack of trust in fellow teammates and clinic systems is negatively impacting patient care and clinic culture.
This lack of trust reinforces a culture of reactive individual doer-ship rather than a trusting, engaged culture where team members know they can rely on broader systems.
How might we move from a reactive, “just survive” culture where individuals must solve everything on their own to a culture where staff feel they can rely on clinic systems and their fellow team members?
Developing design principles
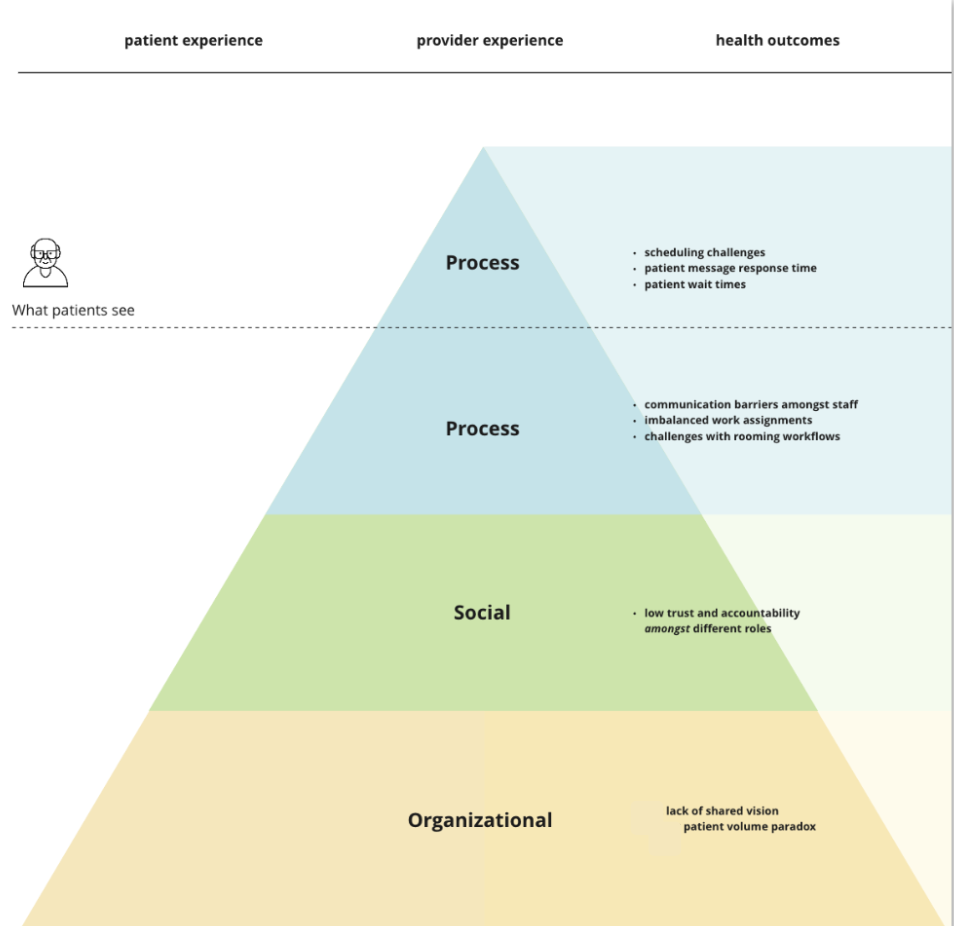
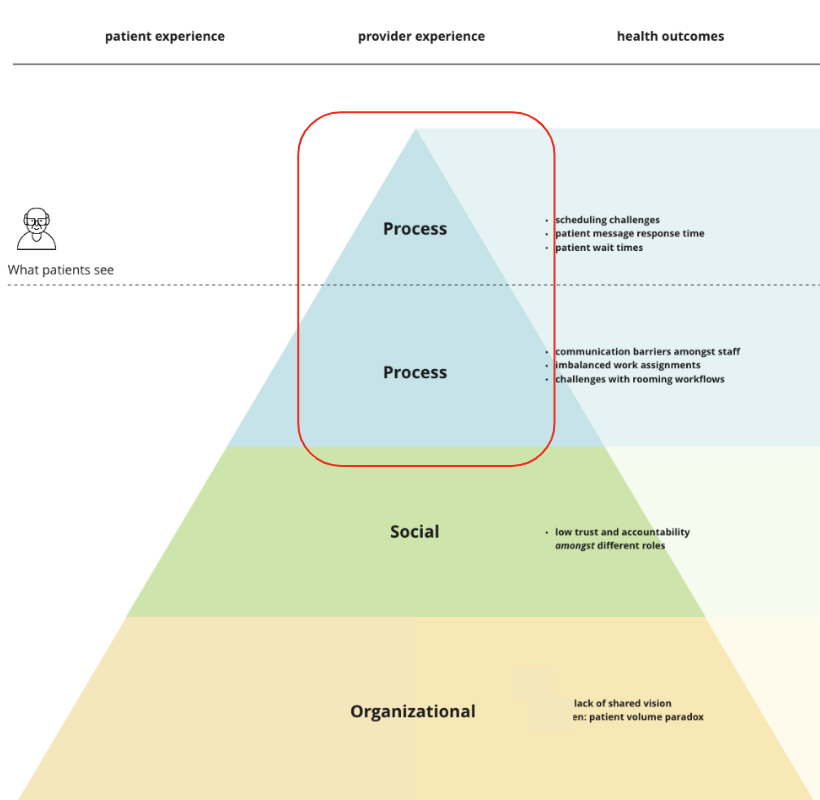
In addition to rebuilding trust in systems and fellow staff, any project proposals needed to also: 1) take place in a realm where HCD could be effective - we chose to focus on process-level challenges (see image on right) such as improving scheduling and message response times, our hypothesis being that more immediate improvements in daily processes would improve motivation for longer-term organizational improvement efforts; 2) honor the lessons learned from previous quality improvement initiatives, meaning any proposed project needed to have: staff buy-in, achievable milestones, an institutionally-informed perspective, a realistic timeline and a plan for long term sustainability; and 3) reflect the desired states shared by staff across roles - in our interviews, staff told us not only about the challenges they experienced but also what they hoped could be different, including a desire for: increased staff capacity and skills, a more consistent internal staff schedule, greater accountability, engagement and trust on teams, improved clinic communication and improved patient services.
Putting these three criteria together with our findings around trust, we knew that any project we proposed needed to meet the following four design principles:
Increase trust in teammates and/or systems
Reflect desired states
Be respectful of clinic partner’s time and past efforts
Ensure a tangible positive impact on daily processes
3. Solution
Solution
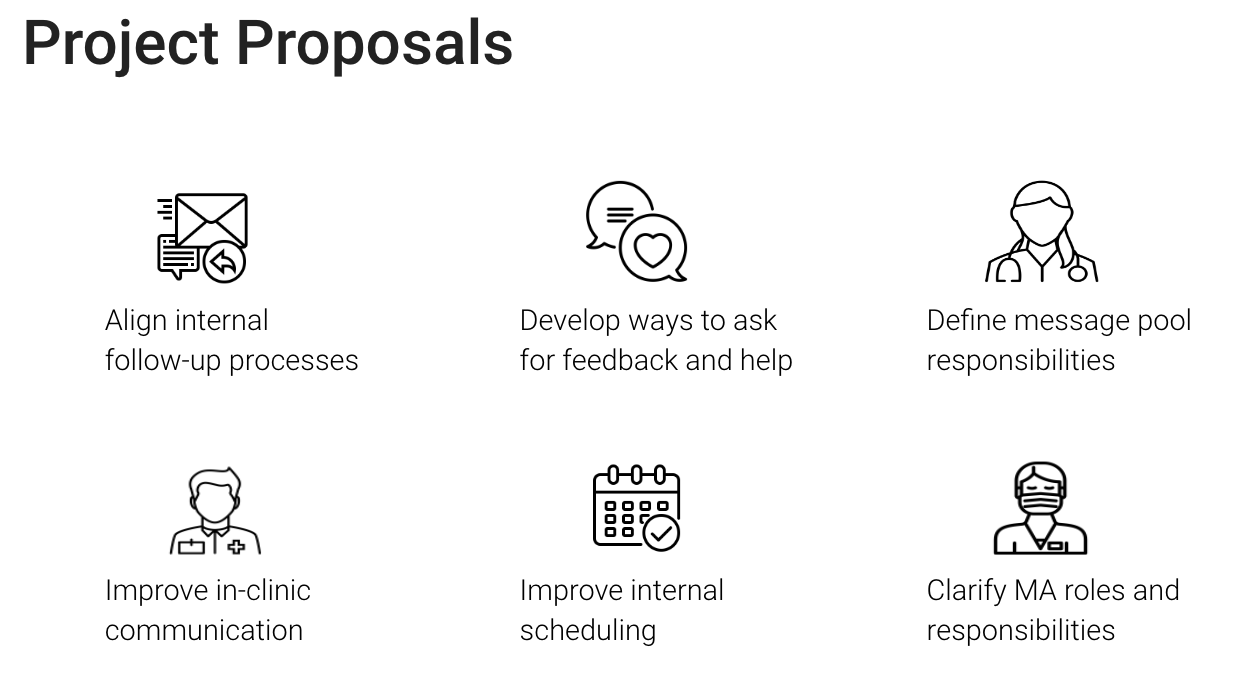
We identified six HCD projects that would address both the key areas of exploration (staff culture, patient experience, patient health outcomes and revenue/patient volume) as well as meet the design criteria (rebuild trust, honor past initiatives, reflect desired states and positively impact daily processes) we had developed through our research.
The clinic leadership was excited about all of these projects and presented the list at their departmental retreat. They chose to move forward with two projects: defining message pool responsibilities and and clarifying the role medical assistants (MAs) play. Both of these projects were appealing because of their potential to tangibly improve multiple clinic processes at the same time. They also were areas that had been having an outsized negative impact on clinic culture for a while and leaders were excited for interventions in those realms.
4. Impact
Client Impact
As a result of our work:
Leaders in this UI Health department walked away from this project with a new understanding of the challenges facing their department. As a result, they were able to make more informed decisions about how to allocate departmental resources in order to address these persistent challenges.
Leaders also got new insights into blind spots of past initiatives as well as exposure to a new set of tools in the form of human-centered design methods, which could be used to address future challenges.
The projects developed through this research have the potential to improve the experiences of hundreds of patients and staff at one of Chicago’s key hospital outpatient clinics.
Personal Impact
It was humbling to work within the institutional complexity of a large hospital system; I learned a great deal from our clinic partners and IHDD mentors about the attitude of incremental change needed to work within such complex systems.
It was also interesting to learn about where HCD is best poised to make an impact within efforts for organizational change (e.g. processes rather than culture). This makes me curious to learn more about other organizational change methodologies that might be complementary to HCD.
Team
Team leads: Emery Donovan + Mona Dong
Project assistant: Archit Potharazu
Advisors: Cam Beversluis + Hugh Musick